EMR Data Migration Practices and EHR Implementation
September 28, 2021Let’s begin this read by properly comprehending the two technical terms EMR and EHR. Although both these digital abbreviations are often used as synonyms, they are two different terms. But, on a common note, both EMR and EHR are aimed at making the healthcare industry cost-effective and efficient.
EMR or electronic medical records refer to the digital presentation of the patient’s chart. Such a chart comprises the treatment and medical history of the person from just one medical practice. EMR reports are mostly stored at a doctor’s office and do not move forward along with a patient if there is a change of doctor.
Whereas EHR software or electronic health records provide a more holistic or long-term view of the patient’s health reports. It is the compilation of all the treatments and medical history from all the consulted doctors to date.
EMR data migration best practices
EMR data migration refers to transferring data between the same or different EMR systems. EMR migration requires careful preparation, planning, and execution of data by following the EMR data migration’s best practices. All of this further requires good communication, complete staff involvement, and proper allocation of time.
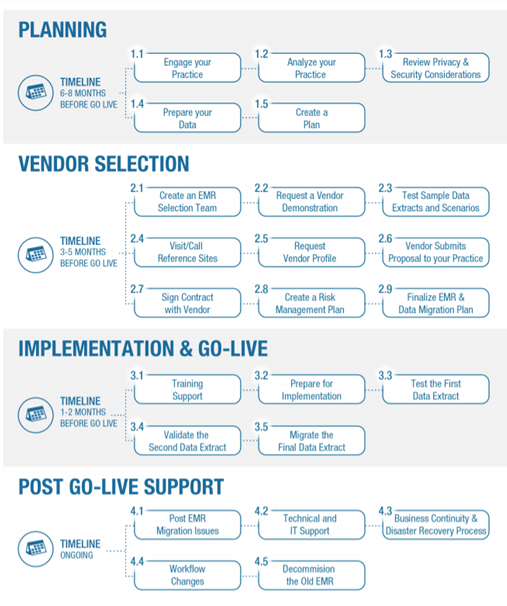
1. Planning
Planning is needed to engage the organization’s staff to curate vendors and EMR evaluation criteria. Planning needs to be done approximately 6-8 months before EMR is scheduled to go live.
2. Vendor selection
Once the workflow gaps functionality has been identified, it’s time for selecting the EMR. The organization can prepare an RFP or RFI report (Request for proposal and Request for information respectively) to compare and finalize the best-fit EMR. Vendor selection takes place 3-5 months before the migration goes live.
3. Data migration goes live
At this point, the setup and configuration of the new EMR and mapping of data are done. Data extraction, testing, validation, and actual migration are carried on. It is done 1-2 months before the actual data migration goes live.
4. Post go-live practices
This involves taking care of:
- Post EMR migration issues
- Technical and IT support
- Business continuity and disaster recovery process
- Changes in workflow
EHR implementation
EHR implementation is the integration of the Electronic Health Records software and its various components in the routine workflow of the healthcare organization. The time taken for EHR data implementation depends on its context, product, and settings. Therefore, it’s not possible to provide a specific timeline for EHR implementation in any healthcare organization. However, few experts provide a rough estimate for the same, after the analysis of all the below-mentioned steps.
Steps to effective EHR implementation
1. Have an EHR implementation roadmap
Any EHR implementation roadmap outlines all the tasks to be executed by the implementation team. The activities outlined on this map are the formation of the implementation team, an outline of the budget and costs, implementation schedule, data migration, EHR testing, go-live activities, and critical success factors.
2. Have an implementation team
The EHR implementation team comprises physicians, receptionists, medical assistants, nurses, administrative and compliance office staff. Clinical team members execute the role of mentoring EHR skills to others and also bring back clinical challenges to the implementation team. The team should have three primary positions – lead physician, lead superuser, and project manager.
3. Forecast the cost and budget of implementation
The cost and budget of EHR implementation depend on the hardware and network upgrades, hiring of temporary staff, temporary loss in productivity, training from EHR vendors, consultancy costs, and finally the cost of data backups and storage.
4. Configure the EHR software
Configure the EHR software to study the security measures. Conduct the HIPAA risk assessment test and customize the software for optimized workflow. EHR software can be customized to design the special physician-friendly template. Discuss the customization options and relative costs of the same with the vendor.
5. Have the right hardware for implementation
Having the right hardware saves a lot of time and money. For example, it’s better to have one common printer for the entire clinic or an exclusive computer system for each employee to save on productive time. The need for system hardware depends on the EHR chosen.
Also Read: Paper Based vs Electronic Medical Records
6. Data migration takes place
The approach for data migration from the traditional record-keeping system to the new EHR should be well-defined. Hire additional temporary staff to execute this step if needed. Maintain a checklist of the information to be transferred. Set an approximate time for task completion by breaking down the entire data into small segments.
7. Start the training program
A successful EHR training program includes super-users as a system and program advocates, a transparent communication system with vendors, training on relevant areas, and space for feedback.
8. Finally, there is a go-live day and post that analysis of the critical success factors.
3 Best practices for EHR Data Migration
1. Have a complete understanding of the data
For successful data migration, a complete understanding of the quantity and quality of data to be transferred is essential. Healthcare data are complex and also abide by high-level security protocols. There is so much inter and intra-organization data interface. For all such reasons, one needs to comprehend the data quality issues much in advance. Failure to do so will cause faulty data migration.
2. Scale up your network and server resources
EHR data migration requires additional server and network resources for a complete setup. Preferably, the healthcare organization should work on expanding its server and network resource during the off-peak time. A plethora of information as data needs to be transferred through the network. All of this does demand time. But not at the stake of downfall in the routine work quality of the healthcare facility. For this purpose, make use of migration tools that increase the data transfer capacity and bandwidth, both at the same time.
3. Choose the best cloud architecture
Opting for cloud-based software is no longer a matter of concern amongst healthcare providers. Owing to its plethora of benefits and with aided cyber security, professionals are now ready for EHR data migration on cloud architecture. But one needs to be careful and use the right tools for proper data integration. Outsource the expertise if needed.
Wrapping up
The process of EMR data migration is not a straightforward task. It involves a lot of technical and functional complexities. Therefore, one needs to hire experts who very well understand the underlying data structure before the actual execution of the task. Beyond the technical understanding, one also needs to abide by some of the mandatory guidelines or practices, which result in the proper execution of the migration process.
